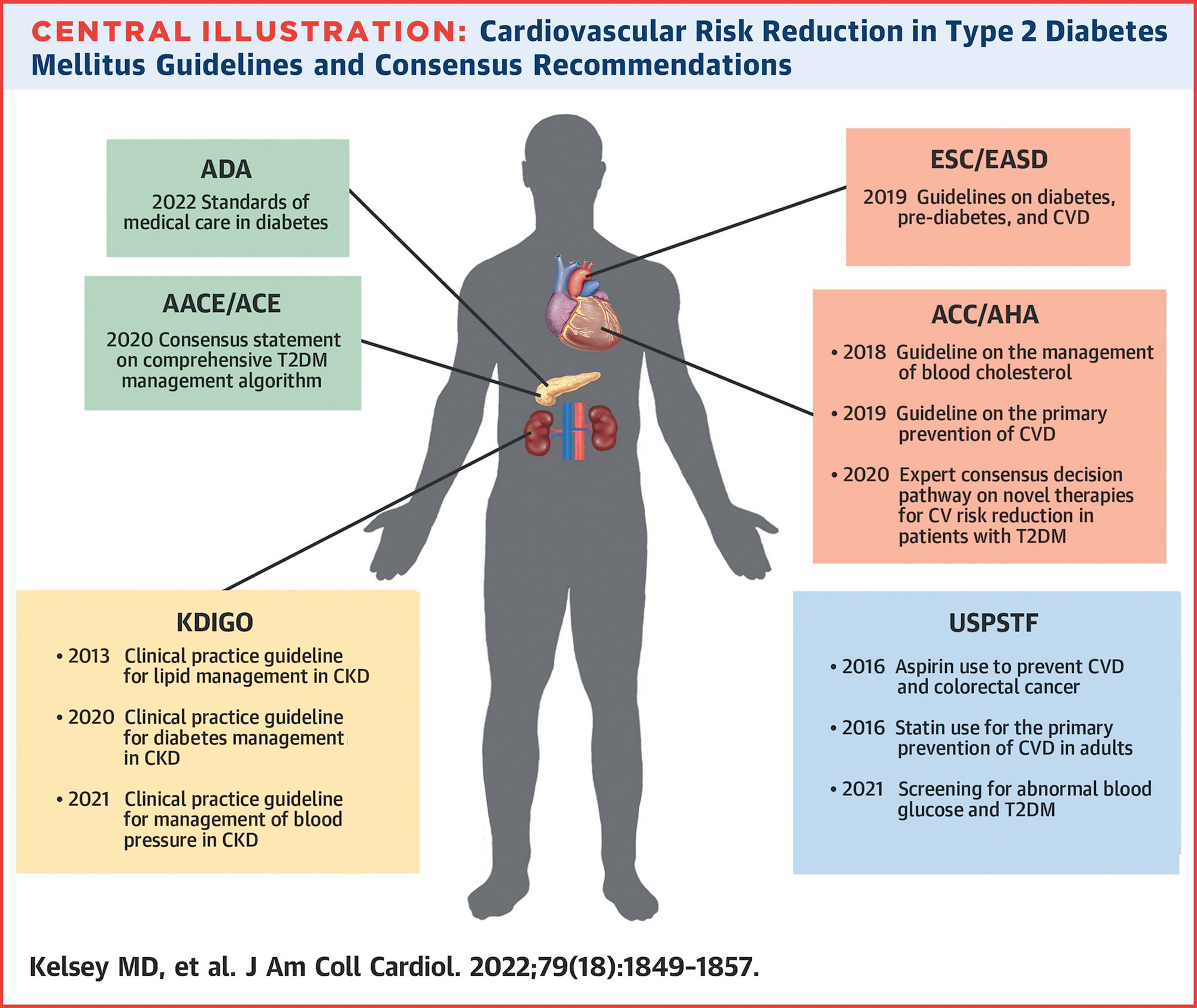
Guideline Recommendations
Source: (Kelsey et al. 2022)
Risk assessment
| Risk assessment method |
Pooled Cohort Equation and diabetes-specific risk enhancers |
Pooled Cohort Equation and diabetes-specific risk enhancers |
Framingham Risk Assessment Tool and risk factors |
Moderate, high, very high risk |
Pooled Cohort Equation |
No recommendation |
Lifestyle modifications
| Exercise |
150 min of moderate-intensity activity per week |
150 min of moderate-intensity activity per week |
150 min of moderate-intensity activity per week |
150 min of moderate-intensity activity per week |
No specific recommendation |
150 min of moderate-intensity activity per week |
| Diet |
Individualized nutrition assessment; Mediterranean Diet |
Individualized nutrition assessment; Mediterranean Diet |
Individualized nutrition assessment; Mediterranean Diet |
Individualized nutrition assessment; Mediterranean Diet |
No specific recommendation |
Individualized nutrition assessment; Mediterranean Diet, 0.8 g protein/day if CKD |
| Vitamin use |
No recommendation |
No recommendation |
No recommendation |
Avoid vitamin supplementation to reduce ASCVD risk in T2DM |
No recommendation |
No recommendation |
BP management
| BP target |
<130/80 mm Hg |
<130/80 mm Hg if 10-y ASCVD risk ≥15%; <140/90 if 10-y ASCVD risk <15% |
<130/80 mm Hg |
<130/80 mm Hg, (but not <120/70 mm Hg), and 130-139 mm Hg in those older than 65 y |
<120/80 mm Hg only for stroke risk reduction |
<120/80 mm Hg if concurrent CKD |
| First-line treatment of hypertension |
ACE/ARB if albuminuria |
ACE/ARB if albuminuria |
ACE/ARB |
ACE/ARB if albuminuria or LVH |
No recommendation |
ACE/ARB if albuminuria |
| Indication for combination therapy |
If BP >140/90 mm Hg |
Dual therapy first line regardless of BP |
If BP >150/100 mm Hg |
If BP >160/100 mm Hg |
No recommendation |
No recommendation |
LDL-C management
| Primary prevention treatment targets |
50% LDL-C lowering for those at high risk |
50% LDL-C lowering for those at high risk |
Numeric goal (LDL-C <55, 70, or 100 mg/dL) |
Numeric goal (LDL-C <55, 70, or 100 mg/dL) |
N/A |
N/A |
| Primary prevention in young patients |
Treat if longstanding disease, end-organ damage, risk factors |
Treat if longstanding disease, end-organ damage, risk factors |
No recommendation |
Treat if LDL-C > 100 mg/dL |
N/A |
N/A |
| Secondary prevention treatment targets |
Goal 50% LDL-C reduction, start meds LDL-C <70 mg/dL |
Goal 50% LDL-C reduction, start meds at LDL-C <70 mg/dL |
LDL-C <55 mg/dL |
LDL-C < 55mg/dL |
N/A |
N/A |
| Secondary prevention second-line therapy |
Ezetimibe |
Ezetimibe or PCSK9i |
No recommendation |
Ezetimibe |
N/A |
N/A |
Hyperglycemia Tx
| First line |
SGLT2i/GLP-1RA may be beneficial regardless of background metformin |
SGLT2i/GLP-1RA may be beneficial regardless of background metformin |
SGLT2i/GLP-1RA may be beneficial regardless of background metformin |
SGLT2i/GLP-1RA first line |
No recommendation |
Metformin and SGLT2i in combination for those with CKD |
| Relative priority of SGLT2/GLP-1RA |
SLGT2i >GLP-1RA for HF, renal disease, weight loss |
SLGT2i >GLP-1RA for HF and renal disease |
SLGT2i >GLP-1RA for HF and renal disease |
No specific recommendation |
No recommendation |
SGLT2 inhibitor first, GLP-1RA second line |
Aspirin recs
| Primary prevention |
May be considered if elevated ASCVD risk without increased bleeding risk |
May be considered if elevated ASCVD risk without increased bleeding risk |
No recommendation |
Not in moderate risk, but can be considered in high or very high risk |
No significant risk reduction with aspirin in individuals with T2DM |
May be considered if elevated ASCVD risk without increased bleeding risk |
CKD
| Type 2 diabetes treatment |
SGLT2i |
SGLT2i, specifically canagliflozin |
SGLT2i |
SGLT2i |
No recommendation |
SGLT2i |
Kelsey, Michelle D., Adam J. Nelson, Jennifer B. Green, Christopher B. Granger, Eric D. Peterson, Darren K. McGuire, and Neha J. Pagidipati. 2022.
“Guidelines for Cardiovascular Risk Reduction in Patients with Type 2 Diabetes.” Journal of the American College of Cardiology 79 (18): 1849–57.
https://doi.org/10.1016/j.jacc.2022.02.046.