Note
Cardiac Arrest
- Work-up
- Labs:
- CMP, CBC, PT/INR, PTT
- Lactate
- Troponin
- If concern for sepsis, check BC x2
- If warranted, beta-hCG to r/o pregnancy
- After intubation and optimize etCO2: check ABG
- EKG
- CXR
- Confirm airway, r/o PNA, PTX, pulm edema
- non-constrast head CT
- Consider pan-scan CT (head, C/A/P) to look for PE or occult foci of bleeding/sepsis
- Echo/POCUS
- r/o PTX, eval for tamponade, hypOvolemia, RV failure, eval for peritoneal ascites/blood
- If concern for PE, consider LE duplex U/S
- Plan
- If concern for MI, consider ASA, P2Y12 inhibitor, heparin/LMWH. arrange for cath
- MAP goal > 75 (2010 AHA MAP goal >= 65)
- Pressors if shock: NE or dobutamine
- Consider stress dose steroids
- Supplemental O2
- Goal sat 94-98% (avoid hyperoxia), PaO2 75-100 mmHg
- Pulm/Crit consult for intubation/vent mgmt
- Goal PetCO2 ~35-40 mmHg; Target PaCO2 40-45 mmHg (2010 AHA Guidelines)
- Keep K > 4, Mg > 2
- TTM if unconsious/unable to follow verbal commands despite ROSC
- Not needed if pt is awake or neuro intact
- Target temp 36 degrees celsius
- TTM options: cold IV saline, ice, cooling blanket
- Continuous temp monitor: bladder/esophageal
- APAP 1,000 mg PO q6h scheduled
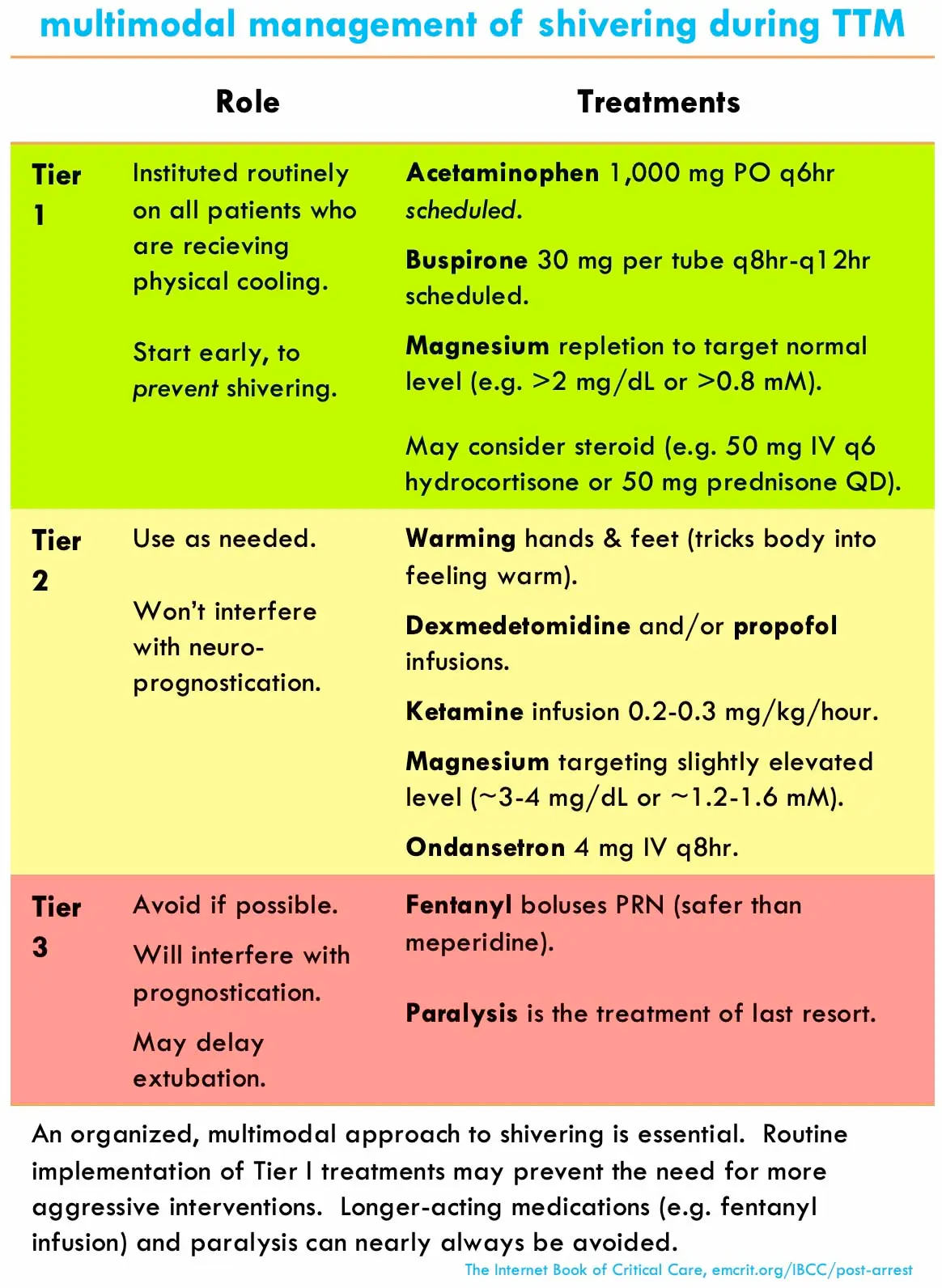
- Multimodal mgmt to control shivering
- EEG
- Tx seizures if evidence
- Consider thorough neuro eval and MRI to assess neurological outcome
- ppx
- DVT ppx
- GI ppx
- Diet: consider enteral nutrition
- Nutrition consult for TF recs?
Manage Shivering during TTM