30 Atrial Fibrillation
If HD unstable or intractable ischemia → immediate DC cardioversion
30.1 Note
Atrial Fibrillation, (*** paroxysmal/persistent/permanent)
- Echo: ***
- CHADS2-VASc score: ***
- HAS-BLED score: ***
- R/R control: ***
- Goal resting HR < 110 bpm (if Asx and preserved LVEF) [RACE II trial]
- Goal resting HR < 80 bpm for Sx AF mgmt despite "lenient" rate control [RACE II trial]
- If recent Dx (within 1 yr), consider rhythm control [EAST-AF trial]
- Anticoagulation: ***
- Indicated if no significant bleeding risk and CHADS2-VASC >= 2 (men), >= 3 (women)
- If CKD 5/ESRD -> warfarin or apixaban (5 mg BID unless TBW < 60 kg or Age > 80 yo)
- Consider checking TSH/fT4, Lytes (inc Ca, Mg)
- Treatment of other co-moribidities
- OSA, HTN, Obesity, EtOH use disorder
- Encourage weight loss (if obese) and abstinence from alcohol (Voskoboinik et al., NEJM 2020)30.2 Classifications
- Paroxysmal - terminates spontaneously or with intervention in < 7 days; recurrence may occur
- Persistent - continuous AF lasting > 7 days; requires termination by cardioversion/ablation
- Permanent - AF > 7 days; sinus rhythm not possible, refractory to cardioversion
30.3 Anticoagulation
Avoid DOACs in patients with mechanical ❤️ valves (RE-ALIGN).
- DOACs for AFib
- Dabigatran: RE-LY
- Rivaroxaban:ROCKET-AF
- Apixaban: ARISTOTLE
- Perioperative management: often we do not need to bridge AC peri-procedurally. (Douketis et al. 2015, 2019)
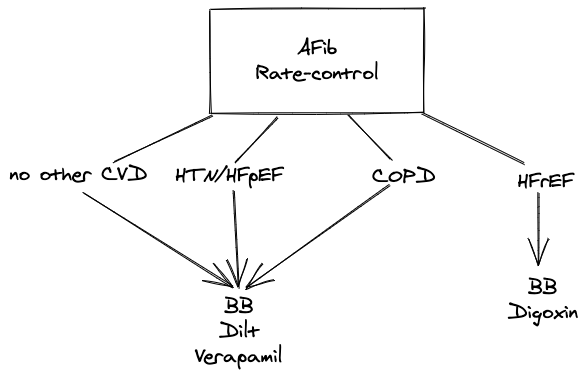
30.4 Rate Control Drugs
- Metoprolol tartrate: up to 200 mg BID
- Metoprolol succinate: up to 400 mg daily
- Carvedilol 3.125-25 mg BID
- Bisoprolol 2.5-10 mg daily
- Diltiazem (extended-release) 120-360 mg daily
- Digoxin: TODO
European Society of Cardiology and NICE guidelines recommend combination therapy if a single agent fails to control HR
30.5 Rhythm control
EAST-AFNET 4 trial (kirchhof2020?)
Early rhythm control within 1 yr of AF Dx with antiarrhythmics or AF ablation (+ cardioversion of persistent AF) was associated with reduced risk of CV mortality, stroke, HF hospitalization, or ACS hospitalization (compared to rate-control)
30.6 RVR management
- IV metoprolol 2.5-5 mg over 2 minutes every 5 mins (up to 3 doses)
- Dilt gtt (if EF preserved)
- Amiodarone 300 mg over 1 hr, then maintenance over 24 hrs
Formula to convert diltiazem gtt to PO dilt: \(\text{PO} = [(\text{IV (mg/hr)} \times 3) + 3] \times 10\). For example, if rate controlled on dilt gtt at 5 mg/hr → PO = 18 x 10 = 180 mg/day.
30.7 Risk factors
Modifiable risk factors
- OSA
- HTN
- EtOH use disorder
30.8 Drugs that may cause/exacerbate AFib
- See Table 2 in AHA Statement on Drug-Induced Arrhythmias (Tisdale et al. 2020)
30.9 Cardioversion Rules
If AFib d/t thyrotoxicosis, cardioversion is often unsuccessful before restoration of a euthyroid state
TEE + therapeutic anticoagulation → cardioversion → at least 4 weeks of therapeutic anticoagulation (indefinitely if increased stroke risk)
Therapeutic anticoagulation x3 wks → cardioversion → at least 4 wks of therapeutic anticoagulation
If duration of AFib < 48 hrs
If HD unstable → just cardiovert, i.e. don’t waste time w/ anticoagulation
If HD stable → start on VTE-dose ppx before cardioversion