5 Orthostatic Hypotension
Related:
- Syncope (Chapter 12)
5.1 Note
Orthostatic hypotension
- Encouraged to rise from resting position gradually, avoid standing motionless (even if still, tense leg mm.)
- Compression waist high stocking (30-40 mmHg)
- Abdominal binder
- Increase salt consumption 6-10 g/d
- Encouraged water intake 2-3 L/d
- If Sx persist despite the above interventions, consider fludrocortisone (if so, recommend high K diet)
- Alternative pharmacotherapy: midodrine
- Patient instructions and education material provided5.2 Pathophysiology
Upon standing, ≈500 to 1000 mL of blood shifts from the central intravascular compartment to peripheral predominantly venous (capacitance) vasculature (lower extremities and splanchnic bed) reducing venous return. Under normal conditions, there is a slight increase in heart rate with associated venoconstriction and arteriolar constriction preserving systolic, but slightly increasing, DBP, effective venous return and maintaining cardiac output. OH reflects failure of the homeostatic reflex autonomic response to postural change at many potential levels (baroreceptors, autonomic afferents, central processing, autonomic efferents, and peripheral sympathetic receptors). (Fedorowski et al. 2022)
5.3 Exacerbating factors
Source: Table 3 of Figueroa et al. (Figueroa, Basford, and Low 2010)
- Dehydration
- Time of day (early morning after nocturnal diuresis)
- Rising quickly after prolonged sitting or recumbency
- Prolonged motionless standing
- Physical exertion, especially vigorous or isometric exercise
- Alcohol ingestion
- Carbohydrate-heavy meals
- Heat exposure or fever
- Straining during micturition or defecation
5.4 Obtaining and Interpreting Orthostatics
- Great overview on orthostatic hypotension
- Performing orthostatics
- baseline: check BP, HR after pt lying down for at least 5 minutes
- after 1 minute of standing
- after 3 minutes of standing
By measuring change in heart rate (ΔHR) and change in supine (and seated) to standing SBP can differentiate neurogenic from non-neurogenic OH. Neurogenic OH is associated with blunted compensatory HR increase (ΔHR <15 beats per minute). Conversely, individuals with non-neurogenic OH will typically demonstrate ΔHR ≥15 beats per minute within 3 minutes of standing. (Fedorowski et al. 2022)
- Interpreting orthostatics
- positive for orthostasis if ↓ SBP of of ≥ 20 mmHg or ↓ DBP of ≥ 10 mmHg
- for HTN pts, a ↓ of SBP ≥ 30 mmHg may be a more appropriate criteria (Freeman et al. 2011)
- HR response
- if HR ↑ by < 15 bpm after standing → suggests neurogenic orthostatic hypOtension
- if HR ↑ by > 20 bpm after standing → suggests volume depletion
- if HR ↑ by > 30 bpm after standing → suggests postural orthostatic tachycardia syndrome (POTS)
- POTS usually presents with typical orthstatic Sx, but do not meet BP criteria for orthostasis, i.e. little/no ↓ in BP w/ postural ∆
- positive for orthostasis if ↓ SBP of of ≥ 20 mmHg or ↓ DBP of ≥ 10 mmHg
For HTN pts, a ↓ of SBP ≥ 30 mmHg may be a more appropriate criteria (Freeman et al. 2011)
5.4.1 Formula to diff Neurogenic vs Non-neurogenic
\[ \frac{\Delta \text{HR}}{\Delta \text{SBP}} \]
Neurogenic OH more likely if \(\frac{\Delta \text{HR}}{\Delta \text{SBP}}\) < 0.5 bpm/mmHg after 3 minutes standing
Neurogenic OH can be diagnosed accurately by measuring the ratio of the HR increase and dividing it by the fall in SBP (ΔHR/ΔSBP) to provide a marker of cardiac baroreflex gain. A ΔHR/ΔSBP ratio <0.5 bpm/mm Hg after 3 minutes standing indicates a diagnosis of neurogenic OH and discriminates neurogenic OH from non-neurogenic OH with significantly better sensitivity than ΔHR alone. (Fedorowski et al. 2022)
5.5 General recommendations
5.5.1 Be SAFE with OH
- Patient Education Essentials for Living with Orthostatic Hypotension (OH): “Be SAFE with OH.” (Fedorowski et al. 2022)
- S: Symptoms and Supplies
- Recognize your symptoms and discuss these with health care providers and important people in your life.
- Symptoms may include: light-headedness, dizziness, nausea, “foggy” brain, pain across shoulders and neck (in the shape of a “coat hanger” on your upper back), feeling like you are going to pass out, falling, passing out, chest discomfort or shortness of breath with standing.
- What supplies are right for you?
- A water bottle to keep with you at all times so you stay hydrated and can drink extra water if you feel symptoms
- An abdominal binder during the day
- may be helpful if you are able to put it on/take it off
- some people find these bulky to wear all day so wear it when they know they need to be standing for a long period of time
- A walker (or rolling walker with seat and brake) may be helpful if you hold onto furniture to walk or have fallen
- Some people try compression stockings up to the waist during the day (but these must fit properly fitting)
- may be helpful if you have a problem with blood pooling in your legs or if you systolic (top number) blood pressure drops to below 90 mm HG.
- If you use these, put them on in the morning before you get out of bed
- Some people need help or a device to help them apply and remove stockings
- Recognize your symptoms and discuss these with health care providers and important people in your life.
- A: Act on Risks and Symptoms
- At-Risk Activities include:
- getting up during the night and first thing in the AM
- showering, after exercise or hot tubs
- after a big meal especially filled with sugar or alcohol
- after lying, sitting, or standing for a long time without changing positions
- If you drop something, squat to pick it up (instead of leaning down)
- Avoid standing in one place for very long
- Act on symptoms:
- Acting with counter-maneuvers
- Tense your abdominal and leg muscles, bend forward with legs crossed
- Sit and cross your legs and arms
- Pump and contract your leg muscles
- Drink water rapidly
- Acting with counter-maneuvers
- At-Risk Activities include:
- F: Food and Fluids
- Fluids – drinking enough fluids each day is very important. Talk to your health care provider about specific guidelines (e.g., if you have heart or kidney conditions, you may have a limit for fluids)
- Drink fluids throughout the day
- Some people drink a “bolus” 2 cups of extra water (about 480ml or 16oz) before they get up from a lying position, before they exercise, after a meal, or when they feel symptoms
- Food – avoid large, carbohydrate-filled meals
- It may help to eat 3 small meals + 3 snacks a day (instead of 3 large meals)
- Fluids – drinking enough fluids each day is very important. Talk to your health care provider about specific guidelines (e.g., if you have heart or kidney conditions, you may have a limit for fluids)
- E: Evaluate, Educate, and Exercise (Safely)
- Evaluate (check) your blood pressure yourself at home (or have someone help you) using a device approved by your health care provider.
- Ask how you should measure your blood pressure first thing in the morning (or after lying at least one minute), then after standing for 1 minute and 3 minutes).
- However, only take standing blood pressure if you can safely check your blood pressure without risk of falling down.
- Keep track of these recordings and share them with your health care provider. It is helpful if you can also record your heart rate and what you were doing before blood pressure (e.g., exercising, eating).
- Educate yourself by talking with your health care provider or pharmacist
- Review what medications may make your OH worse.
- If you take medications for high blood pressure, your health care provider may decrease the dosage or adjust the timing so you take these before bed.
- If non-drug options do not help your OH condition, talk with your health care provider about medications that may help.
- If you become dehydrated (e.g., vomiting, diarrhea), please contact your health care provider.
- Educate yourself and important people in your life about your OH condition.
- Connect with others through and consider a support group, such as http://www.dysautonomiainternational.org/
- Although we don’t yet have research on mindfulness stress reduction techniques (such as meditation), some patients find these helpful.
- Exercise – in a safe way – should be a goal for you with input from your health care provider.
- Have someone with you when you exercise (or stay connected with a smart phone)
- Drink fluids before and after you exercise, and sit down for 20 minutes after exercising
- Avoid exercising too hard or getting too hot
- Some people can develop worsening symptoms with exercise – talk with a specialist about how to exercise safely, progressing gradually, such as with a reclining bicycle, a rowing machine, or swimming.
- Evaluate (check) your blood pressure yourself at home (or have someone help you) using a device approved by your health care provider.
5.5.2 A to F
Recommendations for patients with orthostatic hypotension: From A to F (Figueroa, Basford, and Low 2010)
“Your physician has determined that you have orthostatic hypotension. This means that your blood pressure drops when you stand up, making you feel dizzy or perhaps even pass out. The following may help.
- A: Abdominal compression
- Wear an abdominal binder when out of bed.
- B: Bolus of water
- On bad days, drink two 8-ounce glasses of cold water prior to prolonged standing.
- B (continued): Bed up
- Sleep with the head of the bed elevated 4 inches.
- C: Countermaneuvers
- Contract the muscles below your waist for about half a minute at a time to raise your blood pressure during prolonged standing or when you become symptomatic.
- Specific techniques include:
- Toe-raising
- Leg-crossing and contraction
- Thigh muscle co-contraction
- Bending at the waist
- Slow marching in place
- Leg elevation
- D: Drugs
- Drugs such as midodrine (ProAmatine), pyridostigmine (Mestinon), and fludrocortisone (Florinef) can be used to raise your blood pressure.
- Recognize that some drugs you take can lower blood pressure.
- E: Education
- Recognize symptoms that indicate your standing blood pressure is falling.
- Recognize the conditions that lower blood pressure, such as a heavy meal, positional changes, heat, exercise, or a hot bath.
- Learn the things you can do to raise your blood pressure.
- E (continued): Exercise
- Avoid inactivity and consider a gentle exercise program.
- F: Fluids and salt
- You need plenty of salt and fluids.”
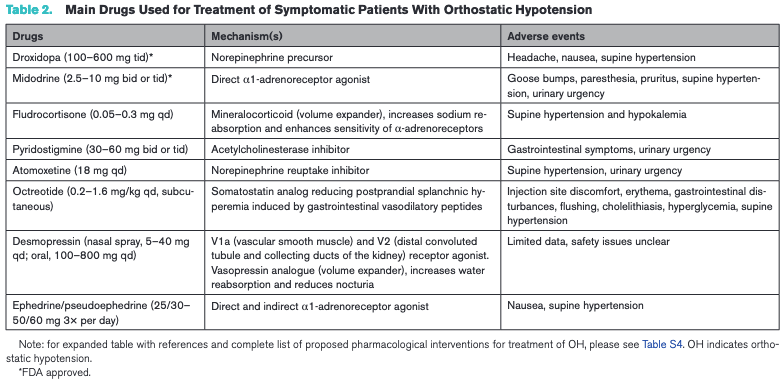
5.6 Pharmacologic Treatment Options
- Midodrine
- A common starting dose is 5 mg three times a day; most patients respond best to 10 mg three times a day.
- As its duration of action is short (2 to 4 hours), it should be taken before arising in the morning, before lunch, and in the midafternoon. To avoid nocturnal supine hypertension, doses should not be taken after the midafternoon, and a dose should be omitted if the supine or sitting blood pressure is greater than 180/100 mm Hg.
- Main side effects are supine hypertension, scalp paresthesias, and pilomotor reactions (goosebumps)
- Ineffective when plasma volume is reduced
- Fludrocortisone
- usual dose is 0.1 to 0.2 mg/day, but it may be increased to 0.4 to 0.6 mg/day in patients with refractory orthostatic hypotension
- a synthetic mineralocorticoid that has a pressor effect as a result of its ability to expand plasma volume and increase vascular alpha-adrenoceptor sensitivity
- helpful when plasma volume fails to adequately increase with salt supplementation and for patients who cannot ingest enough salt or do not respond adequately to midodrine.
- Contraindications: HF and CKD
- The potential risks are severe hypokalemia and excessive supine hypertension. Frequent monitoring of serum potassium, a diet high in potassium, and regular checks of supine blood pressure are advised, especially at higher doses, when added to midodrine, or in elderly patients who tend to poorly tolerate the medication.
- Pyridostigmine
- Dosing is started at 30 mg two to three times a day and is gradually increased to 60 mg three times a day.
- Once daily option: Mestinon Timespan, a 180-mg slow-release pyridostigmine tablet, can be taken once a day
- Can be combined with midodrine: effectiveness can be enhanced by combining each dose of pyridostigmine with 5 mg of midodrine without occurrence of supine hypertension
- most adequate for patients with mild to moderate orthostatic hypotension
- Dosing is started at 30 mg two to three times a day and is gradually increased to 60 mg three times a day.
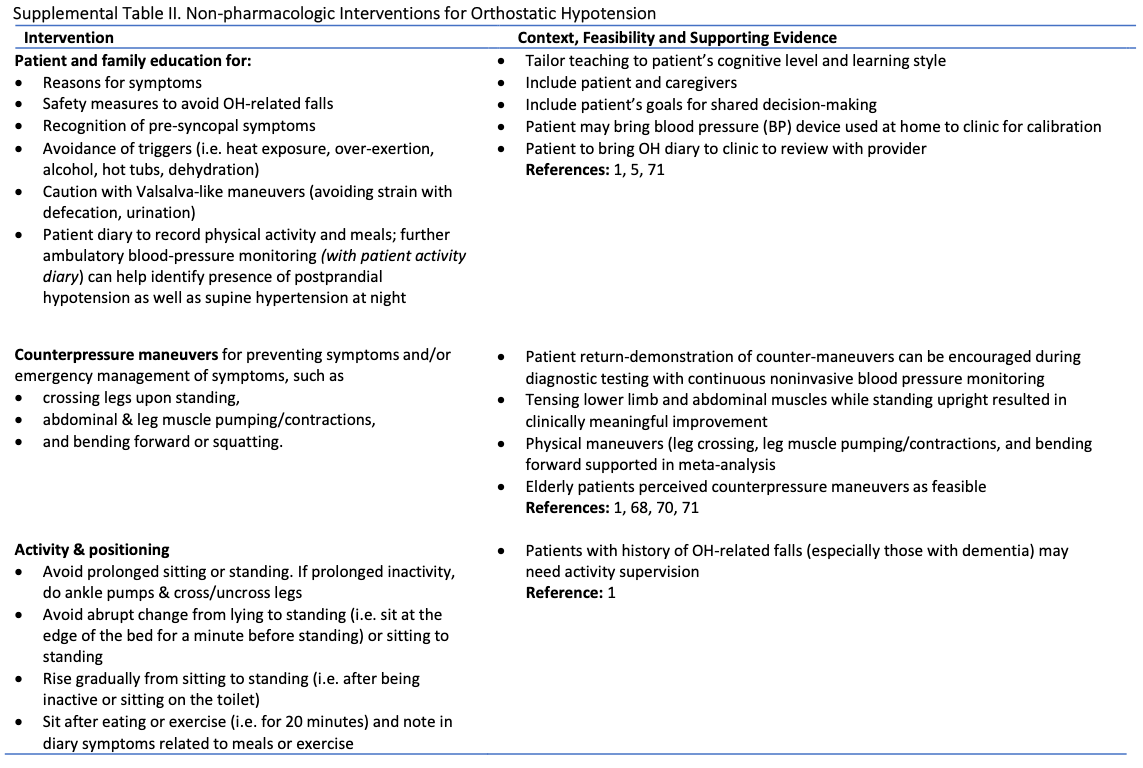
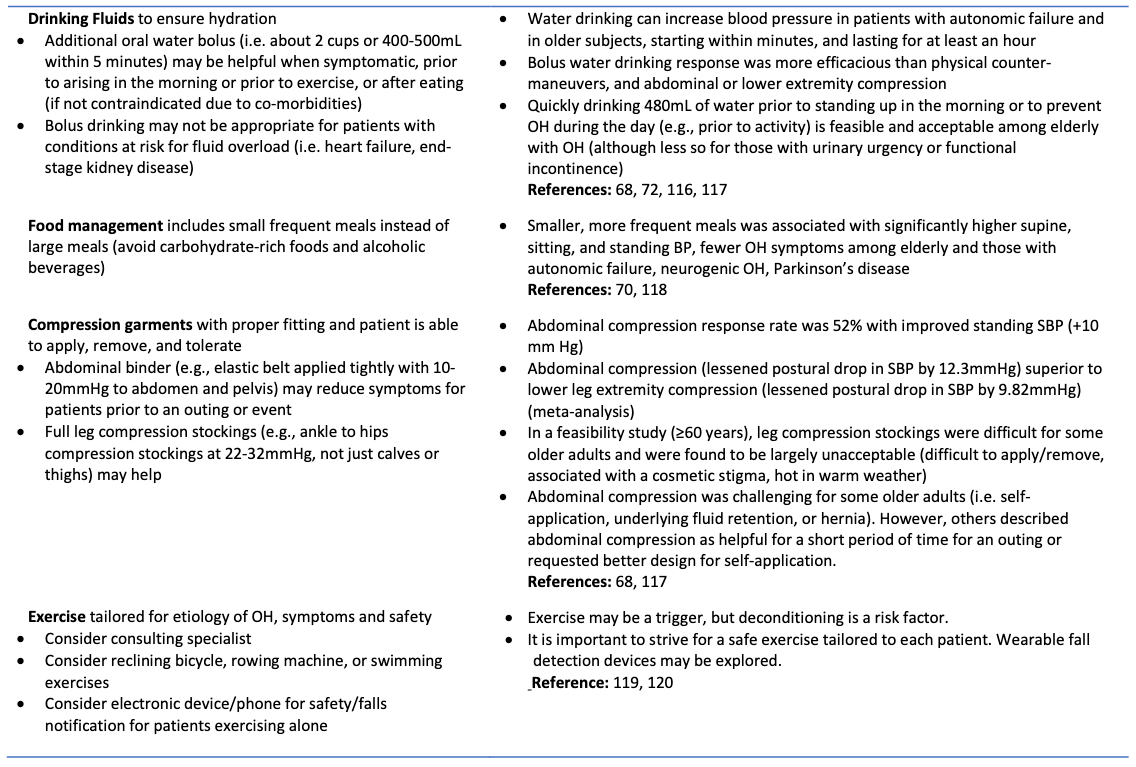
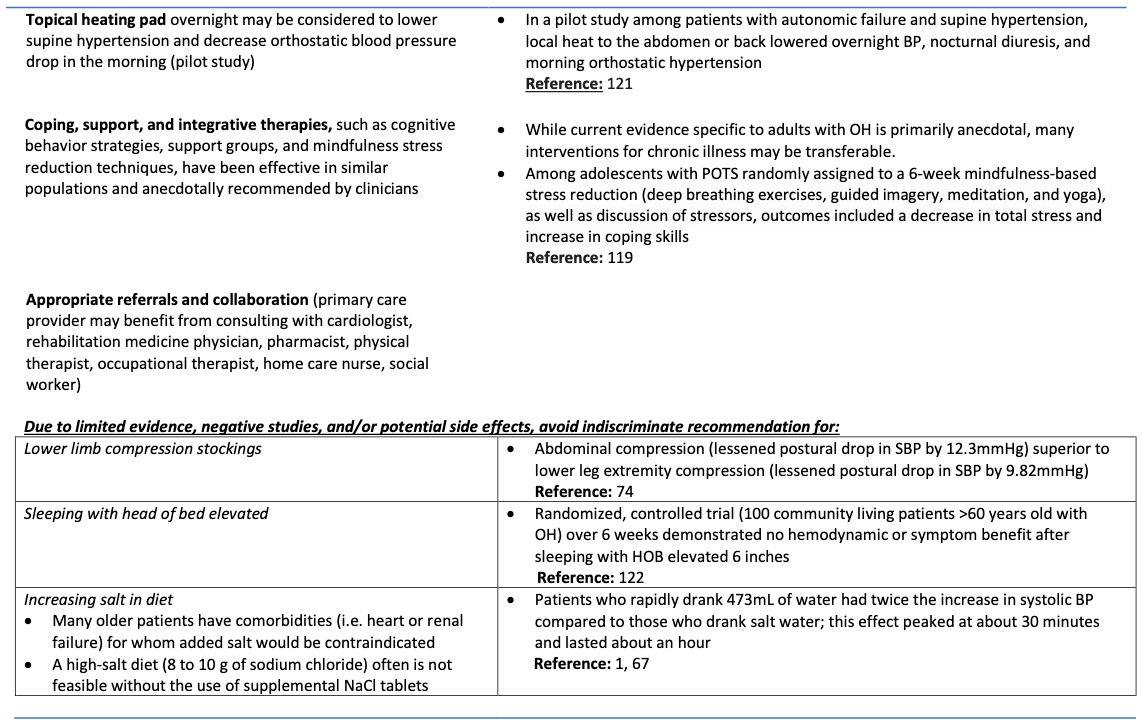
5.7 Non-Pharmacologic Management of Orthostatic Hypotension
5.8 Treatment/Recs based on circumstance of OH
Obtained from Table 1 of Figueroa et al. (Figueroa, Basford, and Low 2010)
- Orthostatic decompensation
- (more severe or less responsive to pressor agents)
- Consider aggravating conditions such as anemia, hypovolemia, heart failure, deconditioning.
- Salty soups and about five 8-ounce servings of fluid over half a day, if acute, or:
- Salt tablets 2 g three times a day with a minimum of eight 8-ounce servings of fluid over 1 day.
- Fludrocortisone (Florinef) 0.2 mg three times a day for 1 week.
- During this time, an abdominal binder can be useful.
- If severe, provide acute hospital management with intravenous fluid expansion.
- Early morning orthostatic hypotension
- Instruct patients to:
- Be careful on awakening
- Elevate the head of the bed (reducing nocturia)
- Drink two 8 oz. cups of cold water 30 minutes before arising
- expands the plasma volume
- Shift from supine to an erect position in gradual stages.
- Instruct patients to:
- Postprandial orthostatic hypotension
- (common in patients with diabetic neuropathy)
- Tell patients to take frequent, small meals and reduce alcohol intake.
- Hot drinks, hot foods, and meals rich in carbohydrates may be troublesome.
- Nocturnal supine hypertension
- Instruct patients to:
- Not take pressor medications after 6 PM
- Elevate the head of the bed to lower intracranial blood pressure
- Try a bedtime snack with a glass of warm fluid (to induce nighttime postprandial hypotension)
- Try a glass of wine at bedtime (for vasodilator effects)
- Remove abdominal binder before bedtime.
- Instruct patients to:
- Anemia in orthostatic hypotension
- (can exacerbate symptoms)
- Mild to moderate normocytic normochronic anemia is not uncommon.
- Consider erythropoietin (Epogen, Procrit) 50 units/kg subcutaneously three times a week (monitor reticulocytes and hematocrit).
5.9 Medications that ↑ risk of OH
TODO
5.10 Orthostasis in the hypertensive patient
- As stated above: for HTN pts, a ↓ of SBP ≥ 30 mmHg may be a more appropriate criteria (Freeman et al. 2011)
- Thread by Inbar Raber
- Probably shouldn’t reflexively ↓ BP meds: A meta-analysis of 9 RCTs found that in HTN pts, more intensive BP treatment actually lowered the risk of OH (paper)
- Some BP meds can ↑ risk of OH