46 Impella
- Impella microaxial flow pumps are placed fluoroscopically in retrograde fashion through the femoral artery, axillary artery, or ascending aorta
- Blood 🩸 is suctioned from an inlet (located just superior to the catheter’s pigtail in the LV cavity) and then delivered through the Impella outlet, which is seated just above the aortic valve.
- The distal portion of the Impella is a pigtail configuration that is meant to reside in the mid LV approximately ==3.5 cm below the aortic annulus==.
- Uses: high-risk PCI, post-MI shock, ADHF, post-cardiotomy shock, etc.
- Complications
- hemolysis
- pigment-induced nephropathy
- vascular access complications, e.g. limb ischemia, major bleeding
- pericardial tamponade
- MV impingement w/ mitral regurgitation
- thrombosis → device failure
- Two main ways it helps:
- unloading (↓ EDV and EDV) and
- outflow (↑ flow)
- Unloads the LV by continuously drawing blood from LV
- ↓ LV work and myocardial O2 demand
- ↑ MAP and CO
- Improved systemic perfusion and coronary blood flow
- ↓ PCWP
- Reduction in RV afterload
- 5.5 is bigger and runs at lower rpm; less hemolysis than 3.5 or CP
Note
“BiPELLA”: combination of LV and RV Impella support devices
- CP - Catheter diameter is 9 Fr, 14 Fr pump motor
- 14 Fr sheath
- Peak flows up to 4.3 L/min
- Advantages
- Quick Percutaneous placement
- Axillary or femoral
- Disadvantages
- Expensive ($25k)
- Higher vascular complications
- Can move with femoral placement
- More hemolysis and thrombocytopenia
- Difficulty mobilizing
- 5.5 - catheter diameter is 9 Fr, 19 Fr pump motor
- 21 Fr cannula in 10mm Hemashield graft
- Peak flows up to 6.0 L/min (even though its called “5.5”)
- Advantages
- Stable positioning
- Good flows
- No pigtail
- Patient can mobilize
- Disadvantages
- Expensive ($45k)
- Surgical placement and removal
- Expensive ($45k)
- Purge solution is used through the impella catheter
- One or the other - NOT used together
- D5W with 25 or 50 IU/ml Heparin
- D5W with 25 or 50 mEq/L Sodium Bicarbonate
- especially if indication not to use heparin
- One or the other - NOT used together
- Inlet should be approximately 5cm into the LV
46.1 Indications
- Cardiogenic shock
- Treatment of acute MI complicated by cardiogenic shock
- Facilitate high risk PCI
- Cardiomyopathy with acute decompensation
- Postcardiotomy cardiogenic shock
- Off pump CABG
- Hemodynamic support during ablation for VT
- Temporary mechanical support as bridge to VAD or transplant
- Temporary mechanical support as bridge to recovery
46.2 Contraindications
- Presence of thrombus in the LV
- Moderate to severe aortic insufficiency
- Will worsen Al and LV dilation
- Aortic Stenosis with AVA 0.6cm2 or less
- Severe PVD
- May still place axillary or direct aortic approaches
- Presence of mechanical aortic valve
- ASD or VSD
- LV rupture or cardiac tamponade
46.3 Important Numbers
- Goals
- MAP 60-80
- CVP 8-15
- PCWP ≥ 10
- Cardiac Power Output > 0.6
- Distance from aortic valve to Impella inlet
- Impella CP: 3.5 cm from valve to inlet
- Impella 5.5: 5 cm from valve to inlet
- Calculate PAPI if CVP > 16
46.4 To-Do after Impella placed and patient rolls into ICU
- Check to make sure that the Tuohy-Borst valves are locked
- Record the centimeter mark on the cather (record at the mark closest to the Tuohy-Borst valve)
- Check volume status and ensure adequate
- Obtain a baseline echo upon arrival to the ICU (or if suspected catheter movement)
- Check Foley bag for urine color (signs of hemolysis?) and amount
46.5 Preventing Impella Inward Migration
- Ensure slack was removed after positioning the inlet area - 3.5 cm for Impella CP and 5 cm for Impella 5.5 - below the aortic valve annulus.
- Ensure the Tuohy-Borst is tight and note the centimeter mark on the cather.
- Immobilize the leg if the patient is overactive or uncooperative
- Obtain a baseline echo upon arrival to the ICU (or if suspected catheter movement)
- Address positioning alarms
- If you do have to move the catheter to reposition, turn down to P-2
46.6 Malpositioned Impella
- Impella in Ventricle
- Appearance on monitor: flat motor current + ventricular placement signal
- Impella in Atrium
- Appearance on monitor: flat motor current + atrial placement signal
46.7 Handling Device Migration
- Reduce to P2
- Under echo guidance, reposition to 3.5 cm below the AV.
- If fails, then will need to go to the cath lab for repositioning under fluoro guidance
46.8 Persistent Suction Alarms
| CVP ≤ 12 | CVP > 12 | |
|---|---|---|
| Persistent Suction Alarm | Low volume status | Strongly consider Right ❤️ Support |
| No Persistent Suction Alarm | No action | High volume status |
- In both scenarious (continuous or diastolic suction alarms), check RV function using PAPI (PA pulsatility index) or Echo.
\[ \text{PAPI} = \frac{\text{PA}_{\text{systolic}} - \text{PA}_{\text{diastolic}}}{\text{RA pressure}} \]
Important
Check right heart function if persistent suction alarms despite good volume status and correct Impella position.
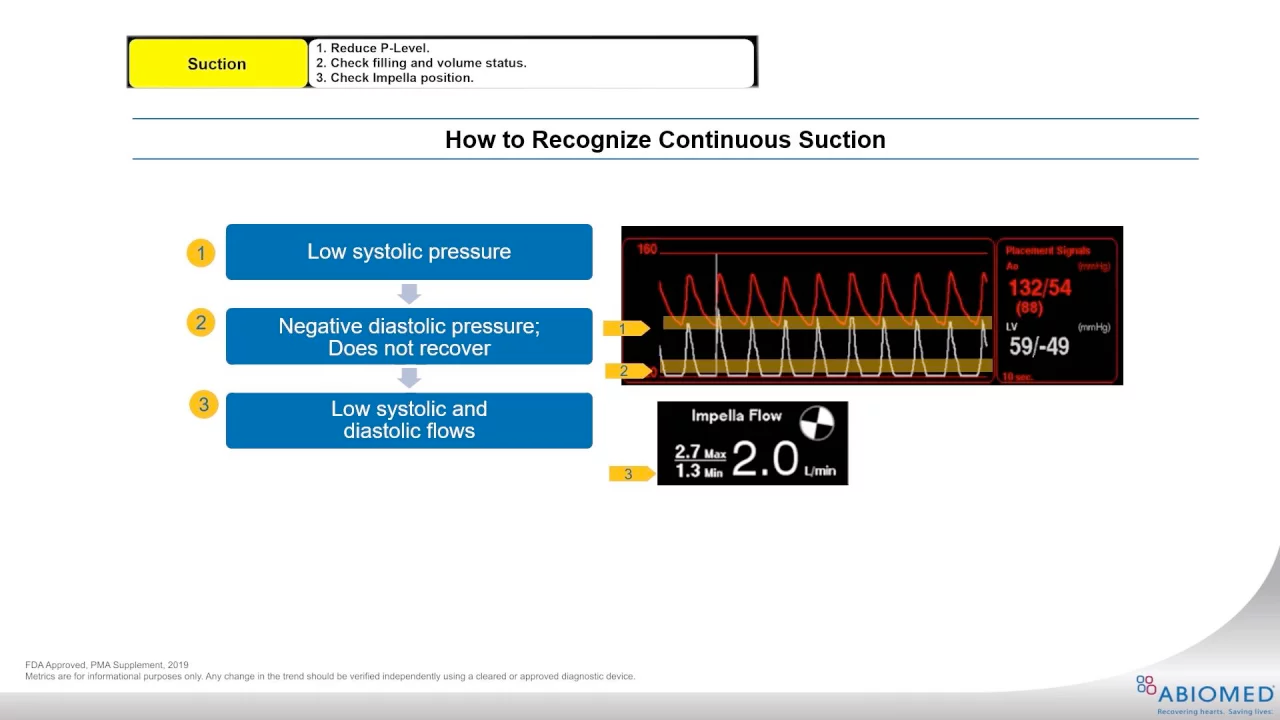
46.8.1 Continuous Suction
- The systolic LV numbers (in white) are uncoupled from the aortic numbers (shown in red). You will see low systolic pressures and negative diastolic pressures that don’t recover (unlike with diastolic suction problems).
- The entire LV waveform shifts downward
- The diastolic LV numbers are also quite negative
- Max and Min Impella flows are lower than expected
- How to resolve?
- Check filling and volume status > Check Impella position
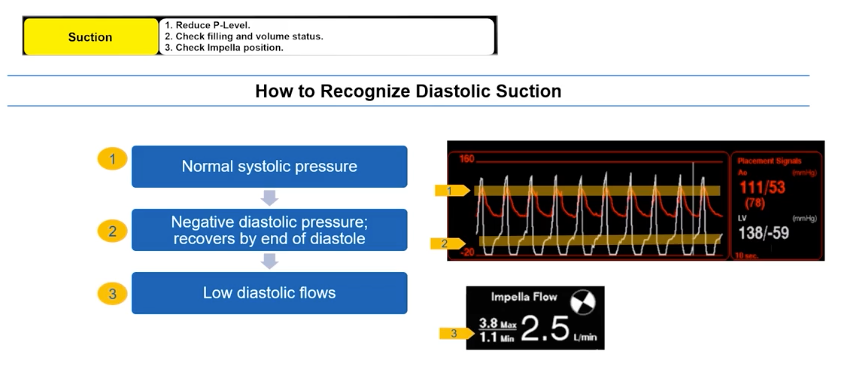
46.8.2 Diastolic Suction
- The LV waveform (in white) will have normal systolic pressures, but negative diastolic pressures that recover by the end of diastole
- There will be low diastolic Impella Flow
- How to resolve?
- Check Impella position > Check filling and volume status
46.9 Handling aberrant purge pressure
- High purge pressure?
- Look for kinks in tubing
- Can ↓ dextrose in purge solution
- Low purge pressure?
- Check for leaks
- Can ↑ dextrose in purge solution
46.10 Bleeding Troubleshooting
- ACT should be maintained between 160-180
- Peel-away sheaths should be removed in the Cath lab
- Minimize unnecessary movement
- Use leg immobilizer to reduce trauma to access site
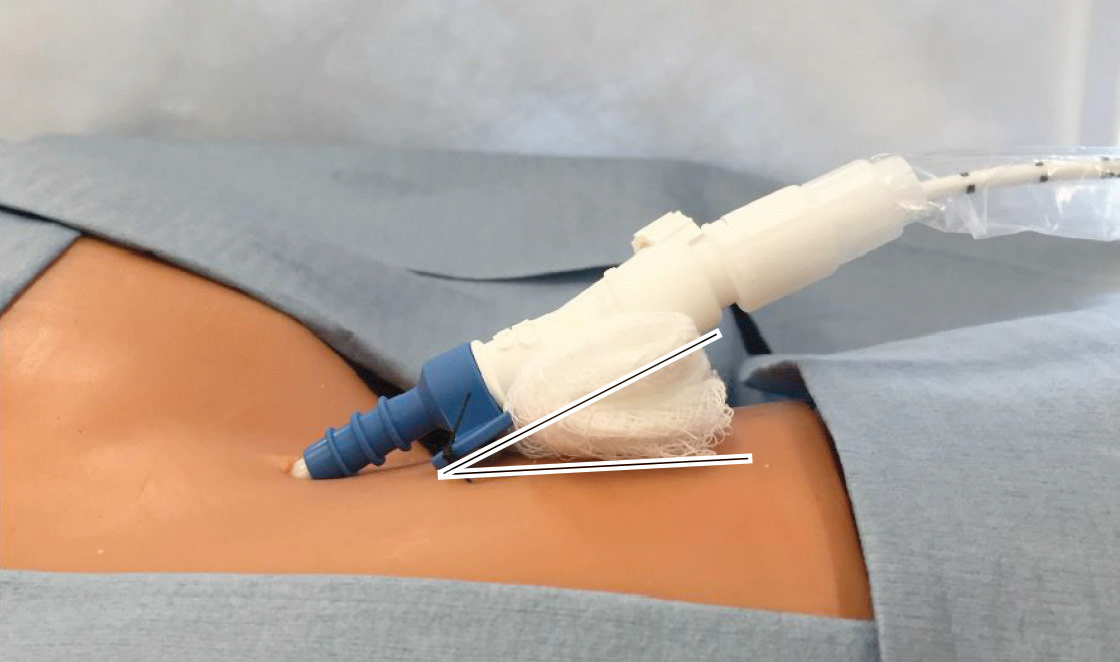
- Check for forward suturing of repositioning unit butterfly
Warning
If butterfly is flat against the skin, use 4x4s to angle match and reduce lift on vessel (See Figure 46.1)
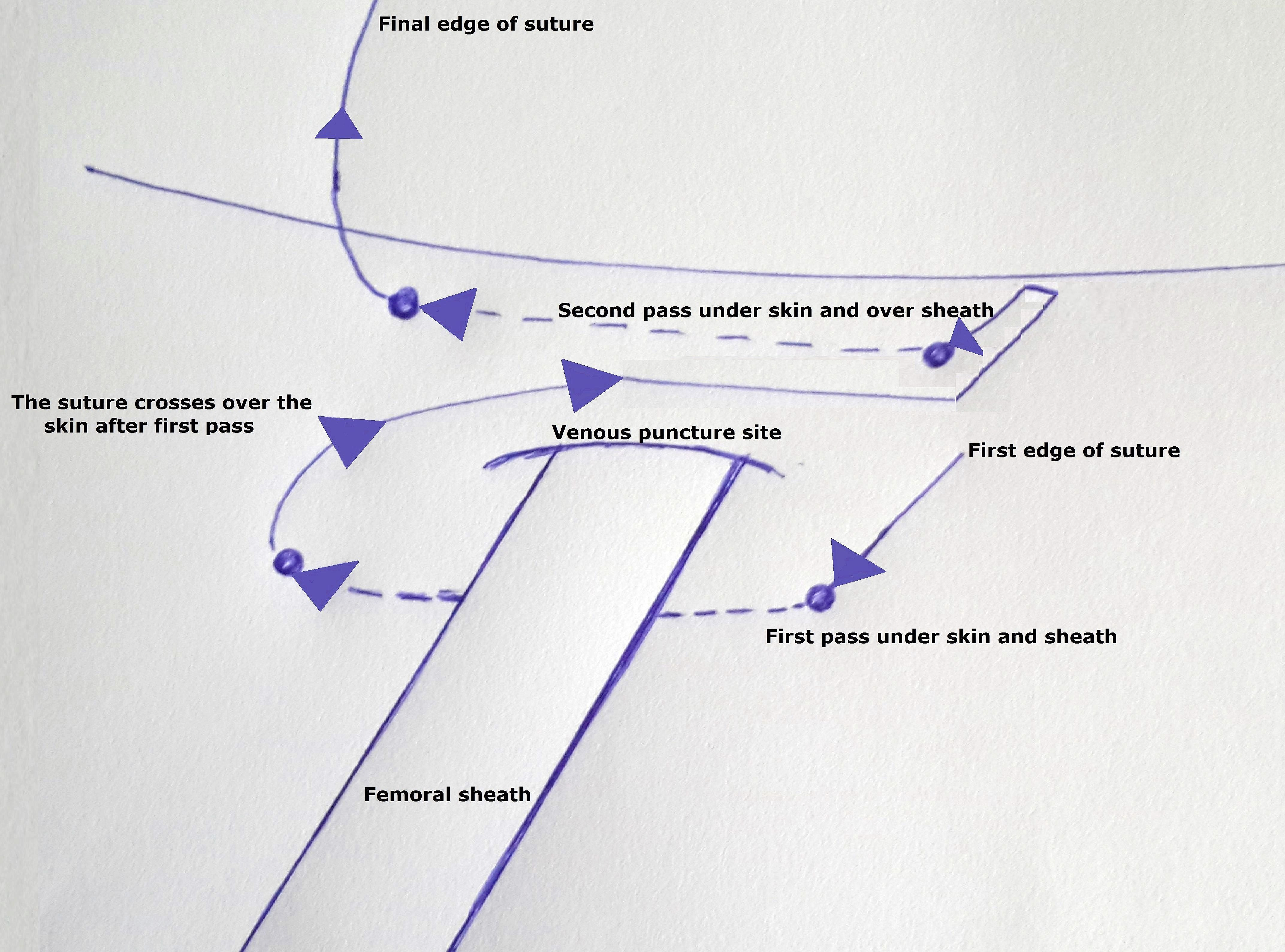
- Dr. Hart also mentioned that the following figure 8 suturing technique may be useful to help with access site bleeding (oozing) (n.d.)
46.11 Suspected Hemolysis
Warning
You should suspect hemolysis if the urine color is red!
- Potential obstruction at different levels
- Inflow obstruction
- Cannula obstruction
- Outflow obstruction
- Rule out blood in urine
- Check a UA (fastest)
- Check plasma free Hemoglobin
- Check spun plasma color if plasma free Hemoglobin is unavailable
- Check LDH
- Consider giving volume if hemolysis + CVP or PCWP < 10 mmHg
- Assess the position of the Impella using Echo
Unobstructed inflow
Approx. 3.5 cm distal to the aortic valve
Free from anterior mitral leaflet
Free from sub-annular structures
Outflow well above the aortic valve
Stable position that does not migrate
Reduce flow as tolerated
Pump removal if needed