25 Heart Failure
25.1 Note
Acute (on chronic?) systolic (or diastolic) dysfunction -
- ACC/AHA Stage ***, NYHA Class ***, Stevenson Profile *** (A, B, C, L)
- *** Exam with S3, elevated JVP, skin is warm, dry
- Presence of ICD/ppm?
- Last EF?
- Work-up:
- EKG:
- Imaging: CXR, Echo
- Labs: BNP, Trop
- Preload: IV diuresis - DOSE trial (2.5x home dose), TDD of home diuretic x2 and give as BID/TID for 48-72 hrs
- If fails to respond, consider adding 5 mg metolazone 1x and reassess
- Afterload: **continue outpatient ARNI/ARB/ACEi/aldosterone antagonist and beta blocker during diuresis if blood pressure allows (Train et al, 2018)
- Neurohormonal:
- R/R:
- Ischemia: statin, ASA
- If pt reports muscle aches: give some oral magnesium oxide
- Diet: salt-restricted diet. If class D HF, consider FWR
- Sodium restriction: 2-3 g daily
- Labs: monitor lytes; maintain K > 4, Mg > 2
- BID labs?
- Monitor HCO3 in COPD pts b/c they can start to retain CO2 (resp acidosis) to compensate for metabolic alkalosis d/t diuresis
- Replete Cl to avoid metabolic alkalosis (esp in COPD pts), e.g. w/ KCl
- Indication for ICD or CRT?
- If HFrEF and *iron-deficiency* (w/ or w/o anemia) defined as ferritin < 100 or
ferritin 100-299 + transferrin sat < 20% -> IV iron for functional and Sx
improvement. Studies of the effect on mortality and hospitalization are ongoing,
as are studies in pts w/ HFpEF.
- If HFpEF - consider spironolactone if elevated BNP, SGLT2i if T2DM
- Encourage lifestyle modifications and optimize co-morbidities
- Daily standing weights
- Strict I/O
- Be mindful of fluids
- e.g. KVO @ 10 cc/hr -> 2.16g Na/d
- 1L of NS contains 9g of NaCl versus 1L of LR contains 6g
- Dispo planning
- Daily home weights; procure weigh scale if needed
- f/u in clinic w/in 1 week of discharge; f/u K, Cr and meds25.2 TODO
- Include JCF paper “A Stepwise Guide to the Diagnosis and Treatment of HFpEF” (Vaishnav and Sharma 2022)
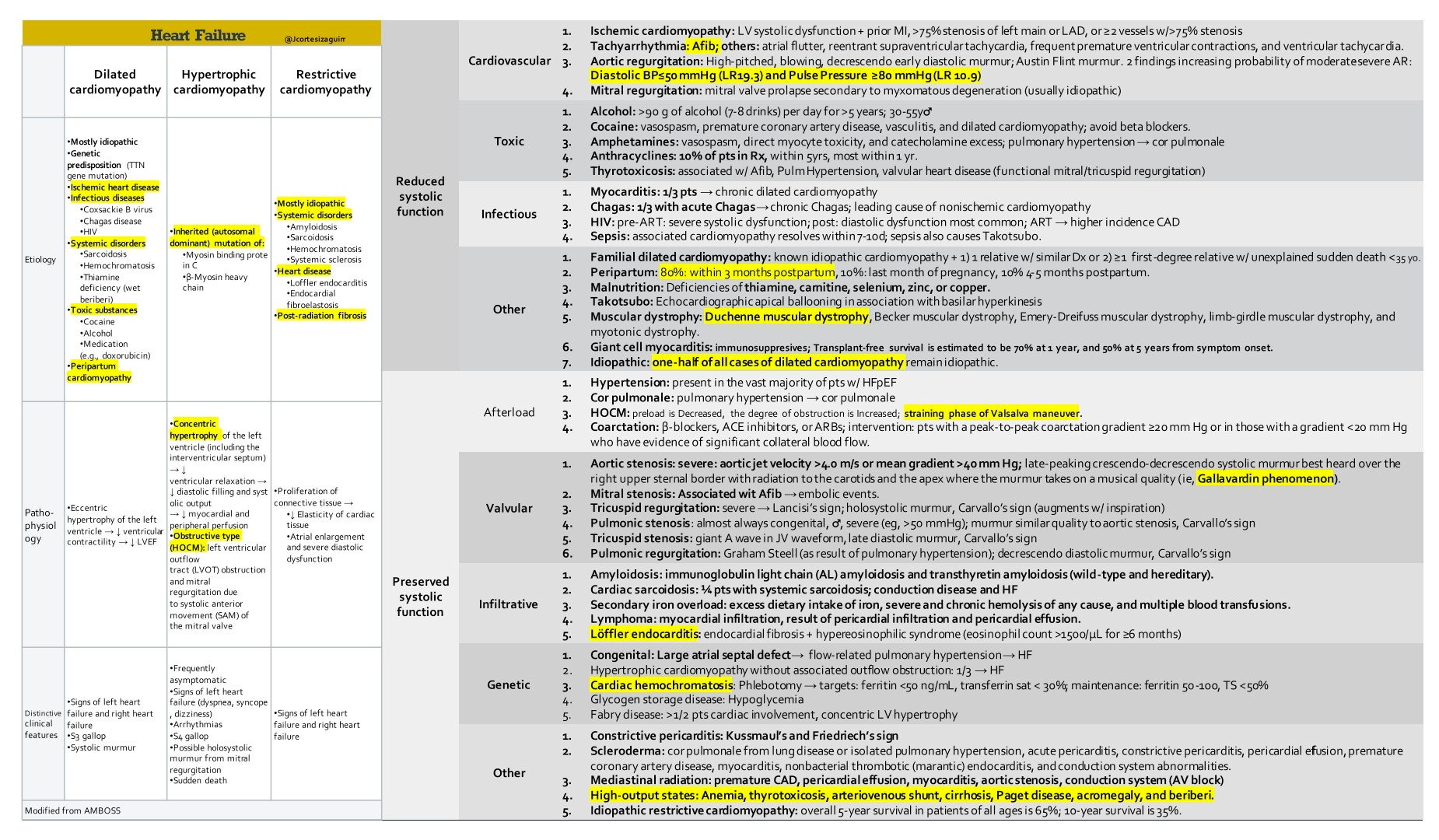
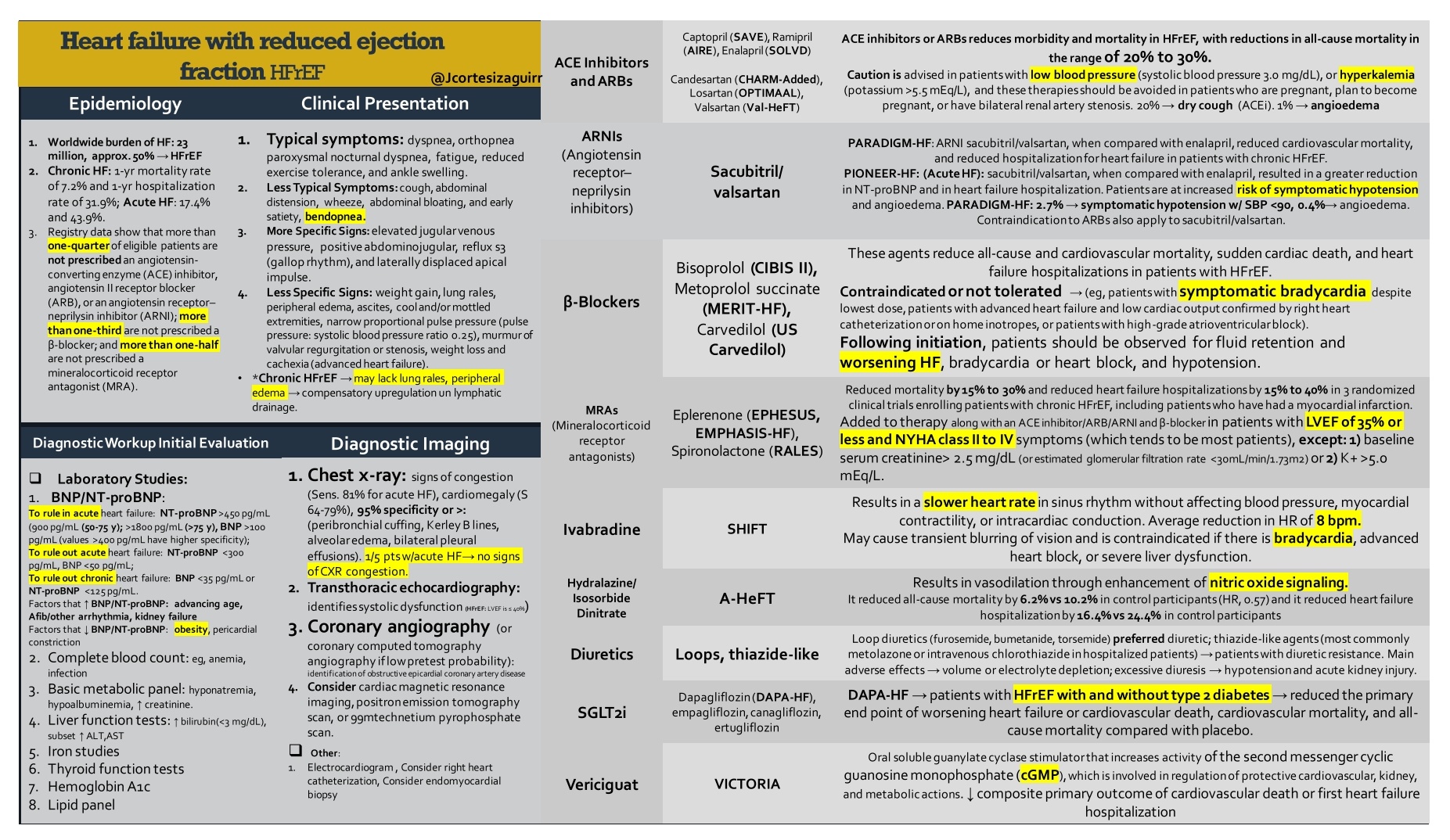
25.3 Classifications of HF
- HF = Si/Sx of HF caused by a structural and/or functional cardiac abnormality plus one of the following:
- elevated BNP
- objective evidence of cardiogenic pulmonary or systemic congestion
- HF with LVEF ≤ 40% (HFrEF)
- HF with LVEF 41-49% (HFmrEF) – HF with mid-range EF
- HF with LVEF ≥ 50% (HFpEF)
- HF with improved EF (HFimpEF)
- Source: Curbsiders tweet from Dr. Yancy’s presentation
25.4 Precipitants of HF
Be mindful of Na+ load from ‘Keep Vein Open’ IVF. KVO w/ NS @ 10cc/hr → 240 mL → 2.16g of Na+. Tweet
FAILURES mnemonic: Source
- Forgetting medication (or taking beta blockers, NSAIDs, methamphetamine, or cocaine)
- Arrhythmia or Anemia
- Ischemia or Infarction
- Lifestyle choices including dietary indiscretions.
- Upregulation of cardiac demand from either pregnancy or hyperthyroidism.
- Renal failure from progression of kidney disease or insufficient dialysis.
- Embolus (pulmonary embolism)
- Stenosis from worsening renal artery stenosis, aortic stenosis, or other valvular disease.
25.5 Work-up
- Exam
- JVD: +LR 5
- Presence of S3: +LR 11
- Work-up for new-onset HF should include:
- TSH
- HIV
- CAD evaluation
- Substance abuse screening: EtOH, cocaine, methamphetamines
- If HFpEF + low-voltage EKG, consider amyloidosis
- Na+ < 125 or ↓ by > 3 during admission is associated with ↑ mortality
Neprolysin inhibitors (ARNIs) can artificially ↑ BNP
- BNP > 100 pg/mL is predictive of HF ( > 200 if AFib)
- Obesity artificially lowers BNP
- Elevators of BNP include female, AFib, ACS, LVH, old age, CKD, etc.
- NT-proBNP < 300 pg/mL excludes HF
- Age cutoffs: < 450 pg/mL for < 50 yo, < 900 pg/mL for 50-75 yo, < 1800 pg/mL for > 75 yo
- EKG
- CXR
- Echo
- RVSP can estimate PA pressure (PASP)
- consider possibility of Pulm HTN in those w/ RVSP > 40 mmHg + dyspnea (ACC/AHA)
- RVSP can estimate PA pressure (PASP)
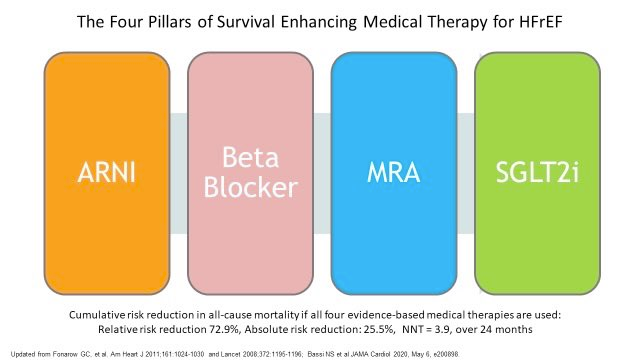
25.6 Medications
- Beta-blockers: metoprolol XL, carvedilol, bisoprolol
- ACEi/ARB
- ARNI - sacubitril/valsartan (Entresto); See Chapter 64
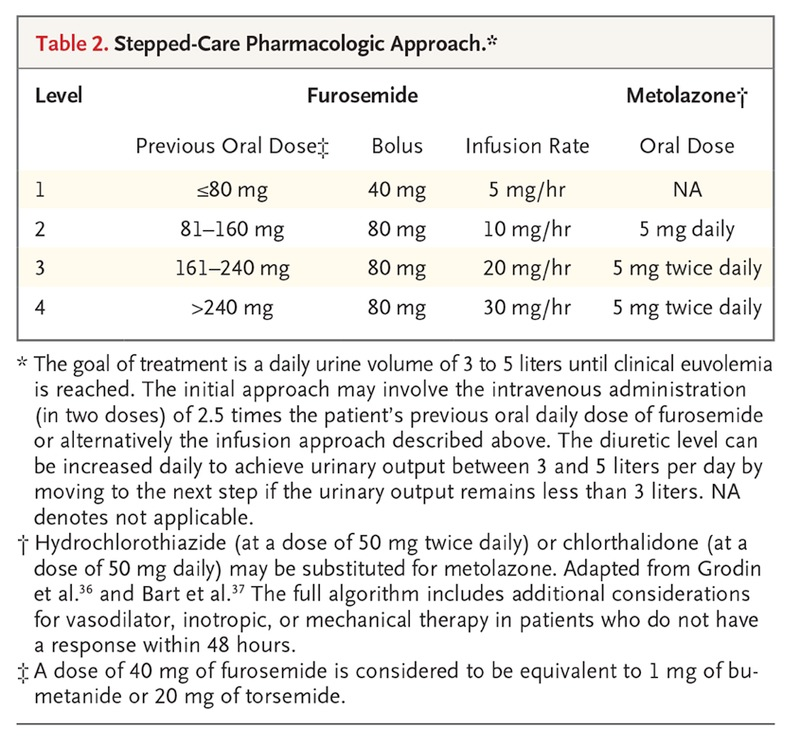
- Diuretics - see NEJM review article
- Goal fluid removal
HFpEF: 1-2L net negative per day
HFrEF: at least 2L net neg per day (“as much as Cr and BP will tolerate”)
If the diuretic response has not begun within a couple hours, increase the dose immediately instead of waiting until the next scheduled dose.
Loops, such as Lasix, Bumex, Torsemide
- Conversions: 40 mg PO Lasix = 20 mg PO torsemide = 1 mg Bumex
- Lasix dosing:
- BUN x 2
- House of God - BUN + age
- Joel Topf - Cr x 20
- Dosing during acute episode - (Clyde Yancy)
DOSE trial - no diff b/w continuous diuresis vs intermittent IV boluses
Clyde Yancy: \(\text{home dose} \times 2\) in IV form administered BID/TID for 48-72hrs
Ellison & Felker bring up a few points about the DOSE trial including: (n.d.)
gtt were not routinely preceded by a loading dose
initial rates of 5 mg/hr (low-dose regimen) and 10 mg/hr (high-dose regimen) are often lower than recommended
- NEJM tidbits:
- PO Lasix bioavailability is highly variable (mean, approximately 50%; range, 10 to 90). By contrast, bumex and torsemide have higher and more consistent oral bioavailability.
- PO and IV doses of bumex and torsemide are equivalent b/c they do not have absorption-limited kinetics
- Torsemide has a longer half-life in pts w/ HF (6 hrs) than Lasix (2.7 hrs) or Bumex (1.3 hrs). Thus, in theory torsemide should be more effective, but the data doesn’t really pan out.
- Torsemide vs. Lasix: Torsemide reduces hospital readmissions for HF (DiNicolantonio 2012)
- Remember that during acute decompensated HF, Na retention is more avid
- Bob Centor gives Torsemide (prefers once daily) to new HF pts and existing HF pts who req’d metolazone during hospitalization. He’ll then Rx metolazone PRN (based on daily weights). (Source)
- Michelle Kittleson recommends transitioning to an oral diuretic dose before discharge that results in 500 cc net negative in 24 hours (expert opinion). Rationale: Patients eat and drink more at home. (Source)
Aldosterone antagonists
- CrCl > 30 + K < 5
- useful in HFpEF pts w/ elevated BNP
- start at 12.5 mg daily w/ repeat K, Cr in 1 week
Metolazone can take > 24 hrs for the effect to be seen (Dr. Ooi)
- Goal fluid removal
- SGLT2i (e.g. dapagliflozin)
- DAPA-HF trial: Among individuals with HFrEF (NYHA 2-4, LVEF ≤40%) with or without T2DM, the addition of dapagliflozin decreased rates of CV death or worsening HF, as well as all-cause mortality. (McMurray et al. 2019)
- FDA approved SGLT2i in pts w/ HFrEF with or without T2DM.
- DAPA-HF trial: Among individuals with HFrEF (NYHA 2-4, LVEF ≤40%) with or without T2DM, the addition of dapagliflozin decreased rates of CV death or worsening HF, as well as all-cause mortality. (McMurray et al. 2019)
- IV iron [FAIR-HF trial]
- if iron-deficiency +/- anemia
- ferritin < 100 or ferritin 100-299 + Tsat < 20% to improve functional status and QoL
- oral iron replacement is not effective [IRONOUT-HF trial]
- if iron-deficiency +/- anemia
- Vericiguat
Resources
- Patient Page: Heart Failure (Baman and Ahmad 2020)
- Association of Optimal Implementation of Sodium-Glucose Cotransporter 2 Inhibitor Therapy With Outcome for Patients With Heart Failure (Bassi et al. 2020)
- Heart Failure With Reduced Ejection Fraction: A Review (Murphy, Ibrahim, and Januzzi 2020)
- The FDA approved use of the SGLT2 inhibitor dapagliflozin for treatment of HFrEF irrespective of diabetes status is expected to become GDMT for all patients with HFrEF in the 2021 ACC/AHA HF guidelines
- Quadruple Therapy is the New Standard of Care for HFrEF (Ahmad and Desai 2020)
- Podcasts
- Tweetorial
- Why can furosemide improve dyspnea/pulmonary edema from acute congestive heart failure within minutes of administration?: 🧵 thread
25.7 Lifestyle Modifications
- Less than 2L fluid or 2g salt per day
- Cardiac rehab
- Exercise: 150 minutes of moderate or 75 minutes of vigorous physical activity
- Smoking cessation
- Decreased EtOH intake
- Sleep apnea Tx
25.8 “Diuretic Resistance”
- Ensure adherence to fluid restriction + low-salt diet
- Ensure pt is not taking NSAIDs
- Maximize loop diuretic dose (Bumex 12.5 mg TID)
- Maximize thiazide diuretic (Metolazone 10 mg TID)
- Maximize other segment blockade (spiro 100 mg TID, acetazolamide 1000mg BID)