18 Chest Pain
18.1 Note
Chest pain, *** typical/atypical/non-cardiac
- HEART score: ***, TIMI score: ***
- EKG
- Labs
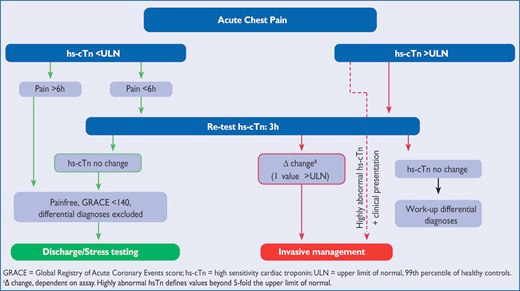
- Trop/hs-Trop - trend q3-4h/1-2h
- BMP, CBC
- A1c
- Lipids
- TSH w/ reflex
- Stress test?
- Consider if clinically stable, no longer having active chest pain and/or non-rising troponins
- ETT/Echo: if pt can exercise/walk on treadmill, BMI < 40
- Nuc perfusion: prior MI, obesity, hx of AFib/arrhythmia
- Dobutamine stress: if hx of lung disease, no arrhythmia, unable to exercise
- ACS protocol?
- Echo?The base rate for myocardial infarction in pts presenting with chest pain is 15%, i.e. about 15% of pts who arrive at the ED complaining of CP are having an MI. ~33% of those patients who wind up getting admitted with suspicion of an MI are actually having an MI.
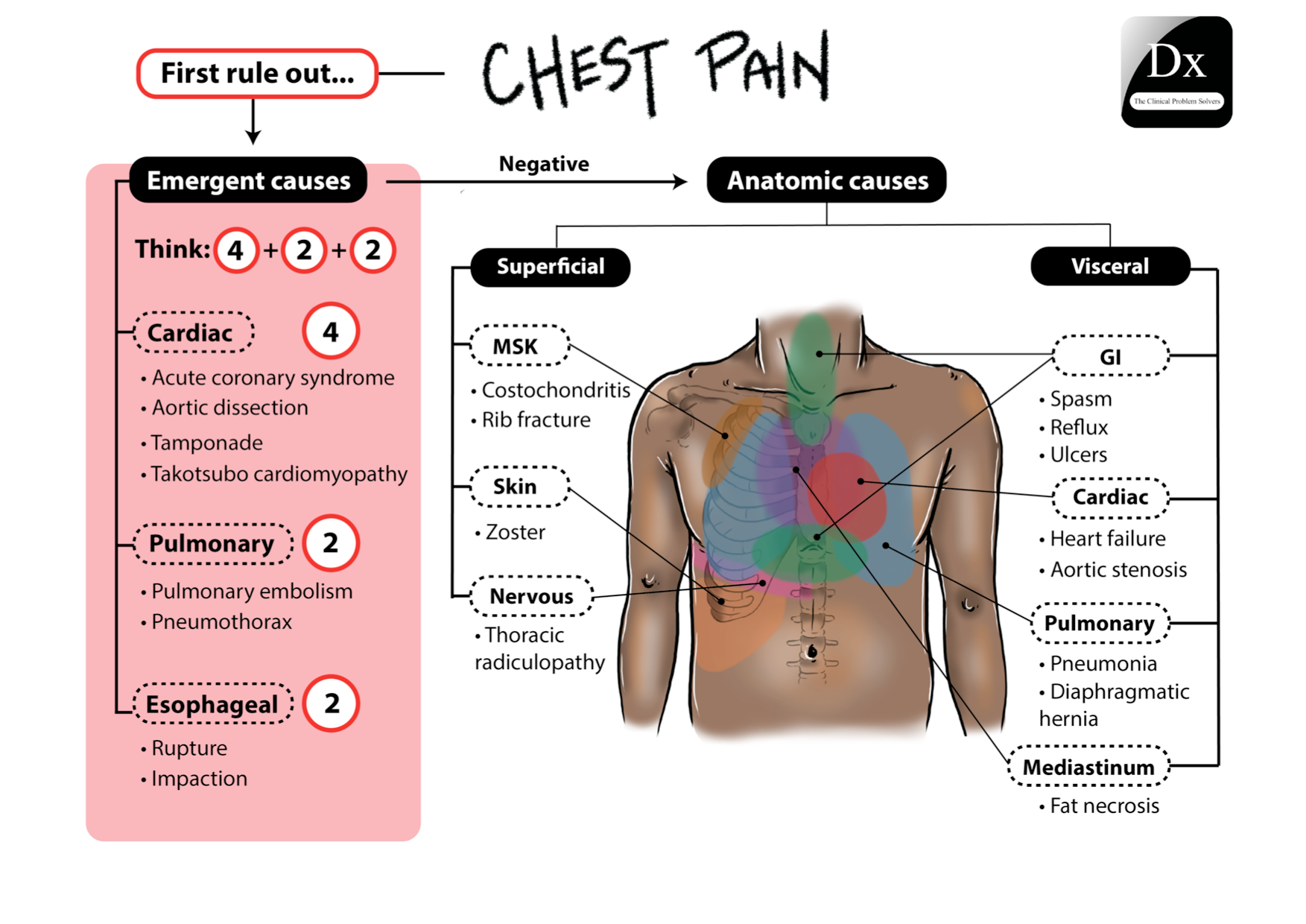
18.2 Serious 6 causes of Chest Pain
Serious 6 life-threatening causes of Chest Pain (PET MAC)
PE
Esophageal rupture
Tension PTX
MI
Aortic dissection
Cardiac tamponade
Other emergenct causes: Takotsubo cardiomyopathy, esophageal impaction
18.3 History Elements
- OLD CARTS
- Hx:
- Description: pressure, burning, aching, squeezing, piercing
- Duration of Sx: acute vs. chronic
- Denied palpitations. radiation of pain, abdominal pain, nausea, vomiting, diaphoresis, or change in appetite.
- Pain is not made worse with deep inspiration or sudden movements. No other palliative or provocative features.
- Denied fevers, chills, cough, no increased sputum production.
- Denied dysphagia, globus sensation.
- Hx that decreases the likelihood of MI:
- pleuritic pain
- sharp or stabbing pain
- positional pain
18.4 Cardiac Risk Factors
- HTN, DM, HLD
- family history
- peripheral vascular disease
- CVA
- CKD/ESRD
- Inflammation/Rheum or elevated inflammatory markers
- Tobacco use
- Recreational drug use: cocaine
- Lifestyle
- poor diet
- sedentary
- obesity
18.5 Clinical Decision Rules
- HEART score
- History, ECG, Age, Risk Factors, and Troponin
- TIMI score
- GRACE score
- Others:
- Patient in the ED with chest pain: Sanchis score, Vancouver rule, HEART score, HEARTS3 score, Hess prediction rule
| HEART Pathway | EDACS | ADAPT (mADAPT) | NOTR | 2020 ESC/hs-cTn | 2016 ESC/GRACE | |
| Target population | Suspected ACS | Suspected ACS, CP >5 min, planned serial troponin | Suspected ACS, CP >5 min, planned observation | Suspected ACS, ECG, troponin ordered | Suspected ACS, stable | Suspected ACS, planned serial troponin |
| Target outcome | ↑ ED discharge without increasing missed 30-d or 1-y MACE | ↑ ED discharge rate without increasing missed 30-d MACE | ↑ ED discharge rate without increasing missed 30-d MACE | ↑ Low-risk classification without increasing missed 30-d MACE | Early detection of AMI; 30-d MACE | Early detection of AMI |
| Patients with primary outcome in study population, (%) | 6–22 | 12 | 15 | 5–8 | 9.8 | 10–17 |
| Troponin | cTn, hs-cTn | hs-cTn | cTn, hs-cTn | cTn, hs-cTn | hs-cTn | cTn, hs-cTn |
| Variables used |
|
|
|
|
|
|
18.6
Risk Stratification
| HEART Pathway | EDACS | ADAPT (mADAPT) | NOTR | 2020 ESC/hs-cTn | 2016 ESC/GRACE | |
| Low Risk |
|
|
|
|
OR
|
|
| Intermediate Risk |
|
NA |
|
NA |
AND/OR
|
OR
|
| High Risk |
|
NA |
|
NA |
OR
|
OR
|
18.6.1
Low Risk by Clinical Decision Pathway
HEART Pathway
- HEART score ≤3, initial and serial cTn/hs-cTn < assay 99th percentile
EDACS
- EDACS score ≤16; initial and serial cTn/hs-cTn < assay 99th percentile
ADAPT
- TIMI score 0, initial and serial cTn/hs-cTn < assay 99th percentile
mADAPT
- TIMI score 0/1, initial and serial cTn/hs-cTn < assay 99th percentile
NOTR
- 0 factors
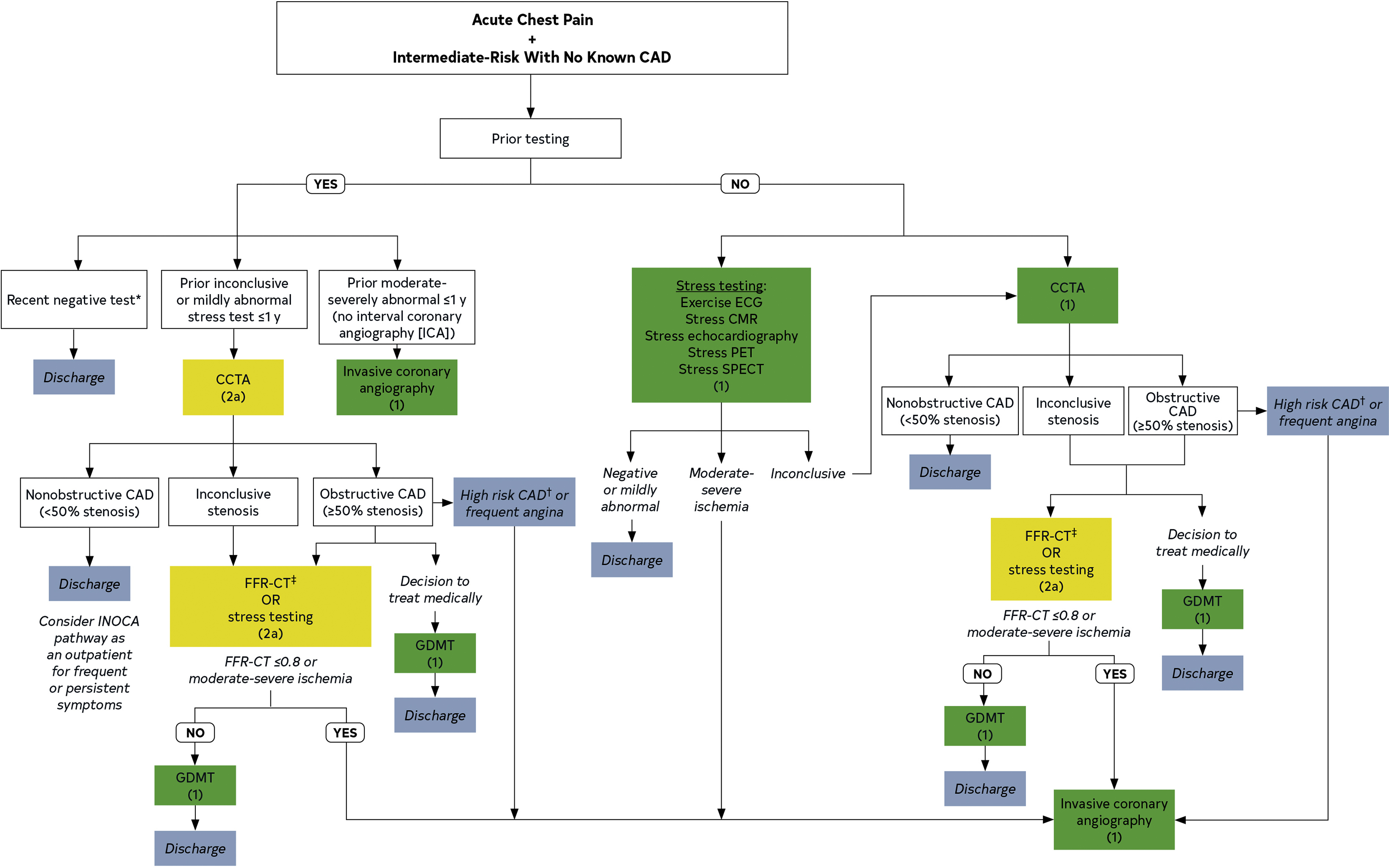
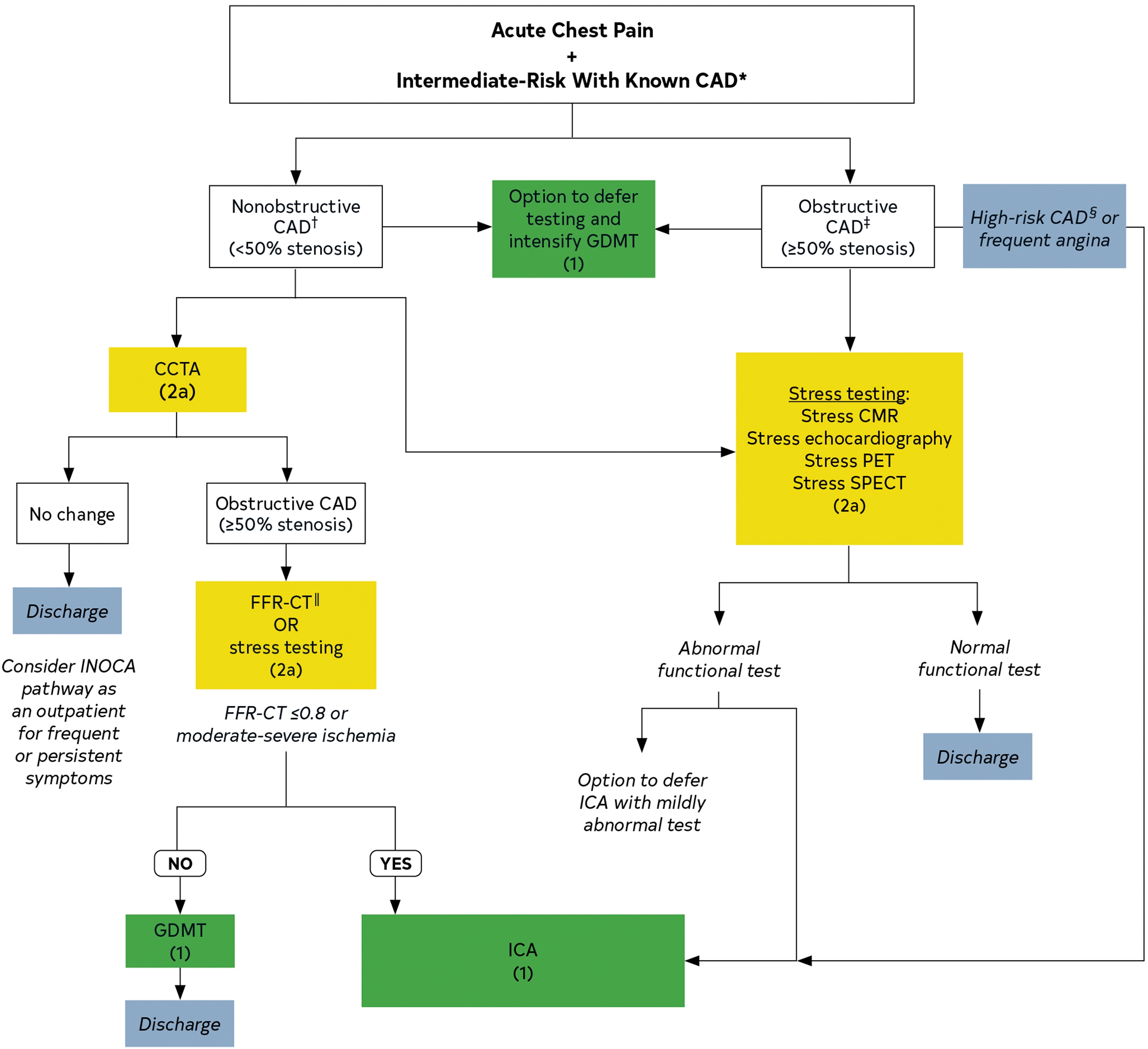
18.6.2 Intermediate Risk Algorithm
18.7 Causes of Chest Pain
18.7.1 Cardiac Causes
- ACS: UA, NSTEMI, STEMI
- Pericarditis/Myocarditis
- Stable angina
- Aortic dissection
- Expanding aortic aneurysm
- Pulmonary embolism
| Classification | Symptoms |
|---|---|
| Typical angina |
|
| Atypical angina | meets 2 of the 3 |
| Noncardiac chest pain | meets 1 or none of the 3 |
18.7.2 Non-Cardiac of Chest Pain
MSK disorders and GERD are common causes of CP that can mimic angina (worse w/ activity, sensation of pressure).
- MSK: costochondritis, rib fx, precordial catch syndrome, Tietze syndrome, pectoral mm. strain, C4-T6 spondylosis, myositis
- Breast: fibroadenomas, mastitis, gynecomastia
- Derm: herpes zoster
- Esophageal/GI: esophageal rupture, esophageal impaction, esophagitis, esophageal ulcer, esophageal spasm, GERD, PUD, malignancy, GB disease, liver abscess, pancreatitis, liver abscess
- Pulm: PNA, PE, pleural effusion, lung mass, mediastinal abnormalities, pericardial disease, diaphragmatic hernia
- Mediastinum: fat necrosis, thymoma, lymphoma
- Referred pain from abdominal process
- Psych: panic, anxiety
- Clues from history regarding esophageal causes of CP:
- odynophagia -> esophagitis, esophageal ulcer
- dysphagia -> GERD, esophageal cancer (RFs include smoking, EtOH, chronic reflux)
- acute pain after retching -> esophageal rupture (Boerhaave syndrome)
- intermittent CP and dysphagia -> esophageal spasm or motility disorders
Study of 100 patients showing prevalence of history findings in cardiac versus esophageal etiology of CP:
| Symptom | Among patients with cardiac cause (%) | Among patients with esophageal cause (%) |
|---|---|---|
| Lateral radiation | 69 | 11 |
| More than 1 spontaneous episode per month | 13 | 50 |
| Pain persists as ache for several hours | 25 | 78 |
| Nighttime wakening caused by pain | 25 | 61 |
| Provoked by swallowing | 6 | 39 |
| Provoked by recumbency or stooping | 19 | 61 |
| Variable exercise tolerance | 10 | 39 |
| Pain starts after exercise completed | 4 | 33 |
| Pain relieved by antacid | 10 | 44 |
| Presence of heartburn | 17 | 78 |
| Presence of regurgitation | 17 | 67 |
| Presence of GI symptoms | 46 | 83 |
“history cannot differentiate esophageal chest pain from pain due to cardiac ischemia. That said, pain that occurs with swallowing, is persistent, wakes the patient from sleep, is positional, and is associated with heartburn or regurgitation is more likely to be of esophageal origin… The effect of nitroglycerin in relieving chest pain has consistently been found to be useless in differentiating anginal chest pain from esophageal or other causes of chest pain.” (Source: Symptom to Diagnosis)